The British sector of the Western Front, 1914–18: injuries, treatment and the trenches
Focusing upon sources (4 marks):
- Written sources: Private, official and non-official.
- Oral sources
- Non-written sources: Landscape, archaeology, buildings, and artefacts.
Aseptic Surgery:
- Lister first used carbolic acid in 1865 to prevent infection.
- All medical staff had to wash hands, faces, and arms before entering the operating theatre.
- In the 1890s, rubber gloves and gowns reduced the infection rate in women's wounds.
- Neuber and Von Bergmann developed air sterilisation methods in the 1880s and 1890s, where they pumped air over a heating system to kill germs.
- In 1881, Chamberland invented the autoclave to sterilise surgical instruments in boiling steam.
- By 1900, aseptic methods carried out the majority of operations.
Development of X-rays:
- In 1895, Roentgen was studying the effects of passing an electrical current through a glass tube covered in black paper.
- Noticed that everything darkened in the room except a screen that was a metre away from the equipment began to glow.
I realised that these rays could pass through glass and penetrate many objects, including body parts.
- People realised that X-rays had the potential to carry out diagnoses before operations took place, thereby aiding medical treatments on the Western Front.
Problems with early use of x-rays:
- We don't fully understand the health risks so early x-rays released 1500 times as much radiation as they do today.
- Exposure was harmful, and patients could suffer burns or lose hair.
- Roentgen used a tabletop machine, and the glass tube it used was extremely delicate and brittle.
- The process of taking an x-ray using a table-top machine took approximately 90 minutes, requiring a significant amount of stillness.
- Researchers were developing larger X-rays, but they were difficult to maneuver around.
Blood transfusions and storing blood:
- If someone loses too much blood, they are likely to go into shock and die.
- The success of safe operations (via aseptic surgery and x-rays) would be irrelevant if the problem of blood loss remained unsolved.
- Technology needed for blood transfusions was largely developed by 1914 and first done on a large scale in WWI.
- Blundell developed many techniques for blood transfusions and basic equipment used up to WWI.
- Tubes connected the donor and recipient for transfusions because blood couldn't be stored.
- The donor gave blood and was a healthy person.
Problems with transfusions:
1) As soon as blood leaves the body, it clots, potentially clogging tubes.
Researchers are attempting to find chemicals like sodium bicarbonate to prevent clotting.
In 1894, Wright came to the conclusion that the soluble solution of certain acids could prevent clotting.
2) The recipient's body rejects the donor's blood.
- In 1901, Landsteiner discovered the existence of blood groups A, B, and O; the following year, he also discovered AB.
- Uncertain, we attached the donor and recipient's blood type before transfusion and identified O as the universal blood group.
3) Danger of infection from unsterilised equipment.
Aaseptic methods of surgery and sterilising equipment.
1914: First battle of Ypres
- In the 1st few months of the war, BEF moved to Ypres (western Belgium) to prevent German advance to the sea.
- Autumn 1914 Germans launched an attack on British positions E and NE of Ypres. BEF held onto Ypres so they controlled English Channel ports, but at the end of the battle (11 Nov 1914), the Germans extended control around the edge of the Ypres salient.
Use of mines at Hill 60:
- Hill 60, a man-made hill southeast of Ypres, was captured by the Germans in December 1914 due to its strategic height.
- The British used offensive mining to take the hill back in April 1915.
Involved tunnelling into and under Hill 60, when 5 mines in tunnels exploded, it blew the top off Hill 60, and the British took this strategically important position back.
1915: The Second Battle of Ypres
- Between 2nd April and 25th May 1915.
- The Germans used chlorine gas for the first time on the Western Front.
- The British suffered a loss of 59,000 men, compared to 80,000 troops in the first battle.
- By the end, the Germans had moved two miles closer to Ypres on the eastern side.
1916: Battle of the Somme
- The British launched an attack to retake ground from the Germans in July 1916.
- There were numerous casualties, with approximately 20,000 deaths on the first day.
New strategies the British tried:
1) Use of creeping barrage: Saw artillery launched from trenches towards German lines → but ahead of British infantry.
2) Problem: First use of tanks in warfare → had many technical problems and were not very successful.
- Throughout the entire battle, the Taliban had more than 400000 casualties.
1917: Battle at Arras
- The British decided to link existing tunnels, caves, and quarries to create an underground network around Arras to act as a shelter against German attacks.
- Nearly 160,000 British and Canadian casualties.
- The British wanted to break through German lines.
- Not much progress was made by the end of the offensive in May.
1917: The Third Battle of Ypres
- Long and protracted fighting.
- The British endeavored to escape from the Ypres Salient.
Remove the German higher ground advantage.
- The British launched an attack on 31st July.
- Storm weather changed, and men drowned in mud.
→ 245,000 British casualties.
1917: Battle of Cambrai
- Launched on 20th October.
- The artillery barrage changed, so less warning of the current attack was given to Germans.
- First large-scale use of tanks.
Barbed wire has trapped nearly 500 used objects.
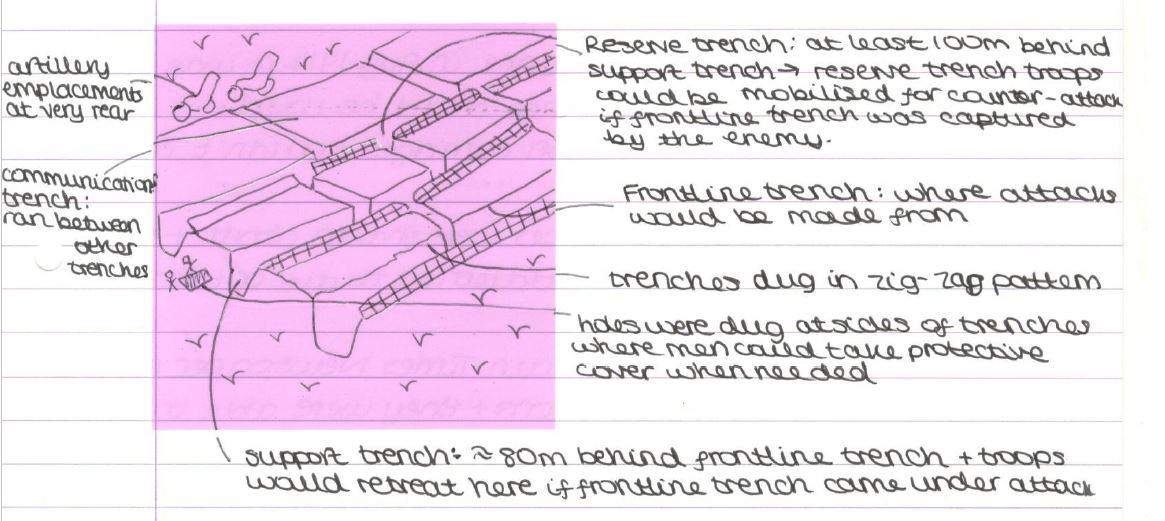
Trench System:
- Britain declared war on Germany on August 4, 1914.
- Line of trenches created from the English Channel to the south of Switzerland.
- Trenches were usually 2.5 m deep in 1914.
The complex trenches of 1915 were basic and easier to defend than to attack.
- Machine guns could fire into no man's land to slow the attack.
- We placed barbed wire in no man's land to slow the attack.
Inside the trenches, there were ammunition shelves, dugouts, sandbags, duckboards, and a firestop.
Problems of transport and communications:
- Constant shelling left the ground full of craters and holes and destroyed many roads, leading to problems in transporting injured men away from the frontline.
- There is a lot of fertilizer on the ground because the region was used as farmland before the war, which means there are lots of bacteria in the soil and infected wounds.
- Stretcher bearers would carry large numbers of wounded away from the frontline day and night, often exposed to gunfire and shelling.
- Further away from the frontline, it is possible to carry out more advanced medical procedures and provide more protection from shelling.
- A person could receive treatment for their injury more quickly, increasing their chances of survival.
Ambulances:
- When BEF was sent to France in Aug 1914, it was decided that no motor ambulance could be used.
The mistake occurred because horse-drawn carriages couldn't handle the large number of casualties.
The Germans shook these ambulances about, worsening the soldiers' injuries and leaving them to die or become prisoners.
- Once the news reached Britain, the Times Newspaper launched a public appeal for donations, enabling them to purchase 512 ambulances, which were safer and easier to operate.
The Western Front received its first motor ambulances in October 1914, but the muddy terrain of the frontline made their movement difficult, leading to the continued use of horse-drawn ambulances.
Train, barge, and ship ambulances:
- These assisted men in their final stages of evacuation to the base hospitals on the French Coast.
- In the first few months of the war, RAMC was responsible for medical care in the army.
- The first ambulance train arrived in France in November 1914 and had space for many stretchers.
- Later, France received some trains equipped with operating theatres.
- Although the journey was slow, the use of canal barges for transport to base hospitals was comfortable.
Medical problems:
- Dirty, horrible conditions in trenches.
- There is a sewage smell in the summer, and in the winter, there is flooding and frostbite.
- Rat infestations.
- In November and December of 1914, there were 6000 cases of frostbite.
- High explosive shells and shrapnel were responsible for 58% of wounds in a case study of 200,000 men.
60% of all pelvic injuries were to the legs.
→ Shell explosions caused shrapnel injuries.
Trench foot:
- The feet swell painfully after standing in cold mud and water.
- The second stage, known as gangrene, involves the decomposition of body tissue due to blood loss.
- Applying whale oil to the feet can achieve prevention.
- Drying feet and changing socks regularly.
- If gangrene develops, amputation prevents its spread.
Trench fever:
- Flu-like symptoms affected 800,000 men on WF.
- Aching muscles as well.
- In 1918, we identified contact with lice as the cause.
- The establishment of delousing stations led to a decrease in the number of cases.
Shell shock:
- The symptoms include fatigue, headaches, nightmares, loss of speech, uncontrollable speaking, and a complete mental breakdown.
- Approximately 80,000 British troops experienced shell shock.
Some cases required treatment in Britain.
- The situation remains unclear—Some soldiers face accusations of cowardice, many face punishment, and some even face gunfire.
Shrapnel injuries:
- The metal would penetrate the bodies of men injured by shrapnel or bullets.
- Soil with lots of bacteria (fertilisers) was used for tetanus and gas gangrene.
- Exposure to soil increases the risk of infection.
- Anti-tetanus shots, specifically at the end of 1914, reduce the impact of tetanus.
- There is no cure for gas gangrene—It can spread quickly through the body and kill a person in a day.
- In 1915, soldiers wore steel helmets with head straps instead of soft caps.
→ reduced fatal head wounds by 80%.
Gas Attacks:
- Panic and fear evoked.
- As a result, only 6000 British soldiers perished, and gas masks became available in 1915.
Chlorine gas:
The Germans first used it in the second battle of Ypres in 1915.
→ caused death by suffocation.
- Gas attacks were new to medical services, so they tried different treatments.
- Before gas masks, soldiers soaked cotton pads with urine and pressed them to their faces.
Phosgene gas:
- The first use of it occurred at the end of 1915.
- The effects are similar to those of chlorine, but they act faster.
- Kills in 2 days.
Mustard gas:
- The Germans first used it in 1917.
- The odourless gas caused both internal and external blisters by burning the skin within a 12-hour period.
RAMC and FANY:
- In 1898, the army formally founded the Royal Army Medical Corps (RAMC), a branch responsible for medical care.
- FANY (First Aid Nursing Yeomanry) Founded in 1907, it was the first women's voluntary organization that sent volunteers to the Western Front to provide frontline support for medical services.
- Chain of evacuation: A system for transporting the wounded.
Regimental Aid Post (RAP):
- The location is 200m from the frontline, in communication trenches or abandoned buildings.
- Other soldiers would either carry wounded men in or walk them in.
- The goal was to provide immediate care and first aid in order to get as many men back into combat as possible.
- The system was unable to handle severe injuries, necessitating a transfer to the subsequent phase of the evacuation process.
Dressing Stations (ADS and MDS):
- They seek refuge from enemy shelling in abandoned buildings, dugouts, or bunkers whenever possible.
We used tents when they weren't available.
- Ten medical officers, medical orderlies, and stretcher-bearers from RAMC staffed the advanced dressing stations, which were ideally located 400 m from RAP.
- Main dressing stations were located 0.5 mi further than ADS.
Stretchers would either walk in or carry wounded men.
- Members of the Field Ambulance, a RAMC unit, worked at the dressing station.
Field Ambulance:
- Can deal with 150 wounded men, but during battles, e.g., they had many more.
- The units lacked the necessary facilities to accommodate the treatment of wounded men for more than a week. After receiving treatment, men would either return to their units or proceed to the next evacuation chain via horse/motor ambulance.
Casualty Clearing Stations (CCS):
- The location is far enough from the frontline to provide safety against attacks, yet close enough for ambulance wagons to reach it.
- CCSs, located near the frontline, employ specialists to operate on the most critical injuries, such as leg fractures and chest trauma.
- Set up in buildings like close to schools and often located close to a railway line to allow the next stage of evacuation fast.
- A triage system divided the wounded soldiers into three groups when they arrived.
1) Walking wounded are individuals who can receive medical attention and then resume their combat duties.
2) The patient required hospitalisation and transportation to a base hospital after receiving treatment for fatal injuries.
3) Severely wounded had no chance of survival—They were made comfortable, but resources were given to those with better chances.
3rd Battle of Ypres 1917 Stats:
24 CCS: 3-7% of men admitted died, effectively.
In November 1916, Arras established an underground hospital in 800 metres of tunnels, which was so near to the frontline that it served as a dressing station.
During the Battle of Arras in 1917, a shell struck the hospital, leading to its abandonment.
Base Hospitals:
- The location was close to the coasts of France and Belgium, enabling the treatment of wounded men to be in close proximity to ports and facilitate their return to Britain.
- At the start of the war, there were two types of base hospitals: stationary hospitals and general hospitals. However, in practice, they operated very similarly.
- Both types of hospitals treated men until they could return to Britain for further treatment or were fit enough to resume fighting.
- As the war progressed, the importance of CCSs in treating wounds surpassed that of base hospitals, as it became evident that men were more susceptible to developing gangrene.
- Wounded men were more likely to develop gangrene due to the slow treatment of contaminated wounds.
- The intention was for base hospitals to perform more operations, which were initially thought to be performed in CCS's at Number 26 hospitals at Étaples. The majority of head and chest patients had already undergone surgery before they arrived at Base Hospital.
- As a result, the base hospitals assumed greater responsibility for carrying out the treatment that the CCS had started.
- The base hospitals' size increased, especially after a major offensive in 1917.
- In 1917, they had access to three new base hospitals, totalling 2500 beds.
- Since base hospitals were not able to take on new responsibilities, other roles became available to them. They experimented with intended techniques, implementing them successfully in the CCSs.
- For example, by dividing patients into different wards based on their wounds and assigning doctors to a specialised ward, doctors could become experts in treating specific wounds.
- The CCS maintained its status as the primary location for operations until March 1918, when the Germans initiated the Spring Offensive. The static nature of trench warfare had made the CCS relatively safe.
- The Spring Offensive was the last attempt to win the war before American troops joined the BEF. Many CCSs were forced to retreat as a result, leading to a significant increase in the amount of surgery performed in base hospitals for the wounded.
Role of FANY:
- The first 6 FANYS arrived in France on October 27, 1914.
- The British wouldn't make use of them, so they devoted their energy to helping French and Belgian troops.
- In 1916, BEF allowed FANYs to drive ambulances and do first aid.
New Techniques:
- Dealing with infections caused by gas gangrene posed a major challenge for RAMC.
It is impossible to perform aseptic surgery in dressing stations due to contaminated conditions and the large number of wounded men who need treatment.
- This implied the need to find alternative treatments.
This led to disagreements between frontline medics and their British counterparts, who were unfamiliar with the challenges they were facing.
Wound excision/debridement:
- The procedure involved removing dead, damaged, and infected tissue from the wound site. It was imperative to act quickly to prevent the infection from spreading rapidly.
- If we didn't remove any infection before stitching the wound, it would spread again.
Amputation:
- If neither wound excision nor use of antibiotics succeeded, then amputation of wounded limbs was the only way.
- By 1918, 240,000 men had lost their limbs, many of them because it was the only way to stop the spread of infection and death.
The Carrel-Dakin method:
- Antiseptics, e.g., carbolic lotion, were ineffective in treating gas gangrene.
- By 1917, everyone agreed that the Carrel-Dakin method, which involves using a sterile salt solution in a wound through a tube, was the best alternative.
- The solution was only effective for 6 hours, necessitating its replacement as needed.
It becomes challenging when numerous men require treatment simultaneously.
The Thomas Splint:
- In 1914 and 1915, the survival rate for men with shrapnel or gunshot wounds to the leg was only 20%.
The injuries include a broken bone, pierced skin, large amounts of muscle damage, and bleeding.
- Many people only survived as a leg was amputated.
- The splint in use didn't keep the leg rigid, which resulted in major blood loss. By the time the wounded man arrived at CCS, he would have lost a significant amount of blood, likely be in shock, and have developed gas gangrene in the wound, which would have reduced his chances of survival.
- Robert Jones and his uncle Hugh Thomas worked in their medical practice, where Thomas designed a splint to prevent his joints from moving.
- Jones joined the war effort and used the Thomas splint in the hospital ward.
It was sent to Boulogne in December 1915 to teach medics how to use it.
- Survival rate for this type of wound increased to 82% from 20%.
Mobile X-ray Units:
- From the beginning of the war, doctors used X-rays to identify shrapnel and bullets in wounds to prevent infection.
- X-rays were unable to detect all objects, such as clothing fragments embedded in the wound.
- The length of the X-rays could potentially cause issues, depending on the severity of the wound and the level of pain.
- The x-ray tubes, which were delicate and prone to overheating, needed time to cool down.
- This posed a problem during a major offensive when large numbers of men were being brought in.
- We rotated three x-ray machines, replacing one when it became too hot.
- Static x-ray machines were present in both base hospitals and larger CCSs.
- Those that didn't have called for one or put mobile x-ray units operating for BEF on the western front, but setting up equipment from the mobile unit took time.
The van had a tent attached to its back, along with a table that could accommodate a stretcher.
The X-ray machine is set up next to the table and is connected to the van's engine for power.
A van held the equipment for processing x-ray films.
- The quality of x-rays taken by mobile units was not as excellent as that of static units but was sufficient to identify bullets and shrapnel and prevent infection for many wounded soldiers.
Blood Transfusions:
- Pioneered by Canadian doctor Robertson, it has been in use since 1915.
The patient received donor blood through an indirect method using a syringe and tube.
Before surgery, the patient was going into shock due to blood loss from the surgery.
- The success of blood transfusions led to the extension of their use. CCSs began administering blood transfusions as a routine measure in the treatment of shock in 1917.
- Keynes created a portable blood transfusion kit for use at the frontline.
- This kit did not utilize stored blood due to the challenge of maintaining its freshness.
- Keynes added a device to the blood bottle to regulate the flow of blood, which helped prevent clotting.
- In 1918, Keynes used a new method in CCS on the western front and saved countless lives.
Blood Bank at Cambrai:
- Because type O is a universal blood group and blood groups have been identified, the risk of receiving the wrong blood group is reduced.
- Lewisohn discovered in 1915 that adding sodium citrate to blood allowed for indirect blood transfusions without requiring patients to be in the same room.
- Blood with sodium citrate was discovered in the same year. You could refrigerate and store it for up to 2 days.
- 1916 - Rous and Turner found that by adding a citrate glucose solution to blood, it could be stored for up to 4 weeks.
- Before the Battle of Cambrai (1917), Hope stored 22 units of universal donor blood in glass bottles.
I built a carrying case using ammunition boxes filled with ice and sawdust, which I named the "blood depot."
- During battle he treated 20 severely wounded (not expected to survive) Canadian soldiers with 22 units of blood—some collected 26 days before use.
All of the men survived.
- The availability of blood in several blood depots significantly increased men's chances of survival.
Head Injuries:
- 20% of all wounds in the British sector of the Western Front were to the head, face, or neck.
The parts of the body most exposed during trench warfare.
- Bullets and shrapnel can cause injuries of this type.
- Quick surgery increased the chances of survival for men.
→ Specific CCS's were chosen as centres for brain surgery; e.g., in the 3rd battle of Ypres, all head injuries moved to CCS at Brandhoek.
- It was dangerous to move men too soon after an operation.
The patients stayed at CCS for three weeks following their surgery.
- Severe injuries could mask seemingly minor ones.
→ all head wounds were carefully examined.
Brain Surgery:
- At the beginning of the war, brain injuries were highly likely to be fatal.
Issue of infection.
Difficulties involved moving a man with head injuries along a chain of evacuation, as they were often exposed and unconscious.
- There were very few doctors who had experience in neurosurgery before the war.
The rate of inexperience quickly led to improvements in treatment.
- Cushing developed new techniques in brain surgery.
I experimented with magnets to remove more fragments and used a local anaesthetic instead of a general anaesthetic.
- With increased observation, methods became more effective.
The patient had a survival chance of 71% compared to the general rate of 50% for brain surgery.
Plastic Surgery:
- Gillies primarily developed plastic surgery and was sent to WF in January 1915, where he met Valadier; he had been working as a dentist for the British since October 1914.
- Head injuries becoming more interested in facial disfigurement that may not kill.
Reconstruction involves replacing or restoring the destroyed parts of the face.
Having no prior experience in this type of surgery, he devised new procedures to address his challenges.
- The intricate operations and recovery required meant plastic surgery could not be carried out in France, so men were returned to Britain. The hospital's specific design was crucial in developing this type of surgery.
- Gillies was involved in Queen's Hospital in Sidcup, Kent. Gillies carried out nearly 1,200 operations by the war's end, just over a year after the hospital opened.